Abstract
Introduction:
Published data reporting gender-related differences in outcomes from sickle cell disease (SCD) is scarce, consisting of small single-center studies. Therefore, using a large sample size from a nationally representative database, we looked into the effect of gender on outcomes from SCD.
Methods:
We investigated the National Inpatient Sample 2019 using International Classification of Diseases-10 (ICD-10) codes to include adult SCD patients. Morbidity, disease complication, and resource utilization were compared, stratified by patients' gender. Analyses were performed using STATA (version 14.2), considering 2-sided P< 0.05 as statistically significant. Proportions were compared using Fisher exact test and continuous variables using the Student's t-test. Confounding variables were adjusted using multivariate logistic and linear regression analyses.
Results:
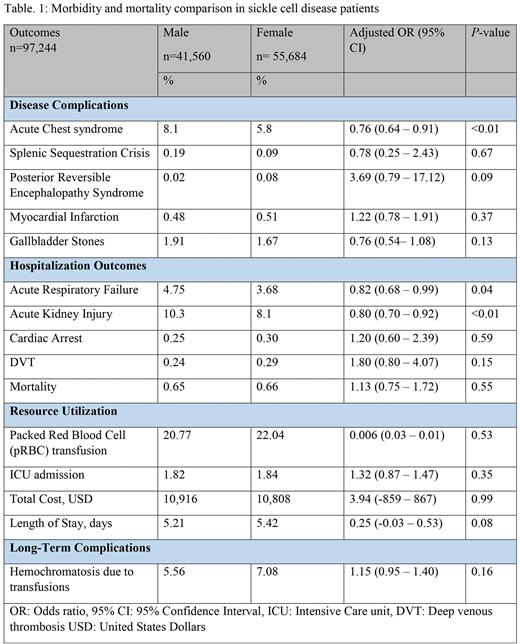
A total of 97,244 patients were included (mean age 34.61 years, 57.26% females). Female patients had 24% lower odds of acute chest syndrome on presentation (Adjusted odds ratio (aOR) 0.76, 95% confidence interval (CI): 0.64 - 0.91, P<0.01). The rates of splenic sequestration crisis, posterior reversible encephalopathy syndrome, myocardial infarction, and gallbladder stones were comparable between the two groups. Males had higher odds of developing acute kidney injury during hospitalization (aOR 0.80, 95% CI: 0.70 - 0.92, P<0.01), but the rates of in-hospital mortality and other morbidity markers were not different between the two groups. Packed Red Blood Cell (pRBC) transfusion, total hospital costs, and length of stay were not statistically different between males and females.
Discussion:
Using a large sample size, we found that females are not at high risk of SCD complications or adverse hospitalization outcomes. Male patients have a higher risk of presenting with acute chest syndrome and developing acute kidney injury. This could be due to the estrogen protective effect or other factors. Despite menstrual losses, females did not have significantly higher pRBC transfusions or lower secondary hemochromatosis. Our study showed that gender does not represent an indicator of morbidity and mortality in SCD.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.